A male infant is born at term with a birth weight of 3.8 kg. His parents are 1st cousins.
They have a daughter age 3 yrs. who is well. There is no family history of neonatal illnesses.
This baby is breast fed and discharged home at 24 hours of age. The following day he is feeding poorly and re-admitted to hospital. On arrival he is lethargic with increased limb tone & some ankle clonus. His weight is 3.3kg.
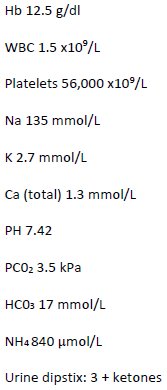
Initial investigations are as follows:
Reference 32 will help you understand this case.
The abnormalities include significantly increased blood ammonia. There is also evidence of bone marrow suppression (low platelet count and neutropenia). It would be unusual to have such a high ammonia with sepsis and an inborn error is consequently probable. The presence of significant ketosis is against a diagnosis of a fat oxidation disorder and with a low bicarbonate is more in keeping with an organic acidaemia, although without further investigations, a urea cycle disorders cannot be excluded.
Results of further tests are as follows:
Bloodspot acylcarnitines:
Urine organic acids:
The acylcarnitine results and organic acids are diagnostic for propionic acidaemia.
The organic acidaemias (OAs), particularly propionic acidaemia, methylmalonic acidaemia and isovaleric acidaemia, commonly present with hyperammonaemia in infancy. Additional clues from the clinical presentation and first line investigations that this may be an OA rather than a primary urea cycle disorder is the finding that the infant is dehydrated, ketotic, and has a degree of bone marrow suppression with hypocalcaemia.
The aetiology of the hyperammonaemia is believed to be inhibition of N-acetylglutamate synthase (NAGS) by propionic acid or other metabolites. Although the OAs are usually associated with a metabolic acidosis, if the ammonia is sufficiently high, the respiratory alkalosis associated with the increased ammonia can initially cause the blood pH to be increased.
For information about the acute management of organic acidaemias see http://www.ojrd.com/content/9/1/130.
N-carbamoyl glutamate (carglumic acid), a structural analog of N-acetyl glutamate, is used for the treatment of NAGS deficiency but has also been given to patients with organic acidaemias (isovaleric, methylmalonic and propionic acidaemias) who have hyperammonaemia. Although there have not been clinical trials to confirm its efficacy, it is generally believed to be an effective therapy.
For further reading regarding the use of N-carbamylglutamate can be found in references 33-39 inclusive.
Learning objectives from this case report:
